Introduction:
The application of novel drugs has significantly enhanced the prognosis of patients with MM. However, most patients will inevitably experience disease progression and relapse. At progressive disease (PD), patients always exhibit distinct features characterized by varying levels of M protein and plasma cells in the bone marrow (BMPC), even in the presence of end-organ damage. Notably, a subgroup of patients initially diagnosed with secretory MM exhibits a higher proportion of BMPC but a lower level of M protein when PD, rendering identification of this subgroup challenging without conducting bone marrow evaluations, leading to many patients experiencing PD but without timely treatment. The identification and comprehension of the hyposecretion at progression remain unclear and require further investigation. Thus, in this study, we aimed to assess the impact of different patterns of disease progression according to M protein and BMPC percentage on the survival and describe the features of the subgroup.
Methods:
We retrospectively analyzed the baseline and progression clinical features of 268 patients in our hospital between January 1, 2013 to July 1, 2023. We classified the PD patterns into three categories based on the elevated level of M protein and clonal plasma cells in bone marrow at progression: a. hyposecretory progression (HypoP) means >10% increase of the absolute percentage of BMPCs but serum M-protein increase <5g/L (or urine M protein increase < 200 mg/24h) and patients with the non-secretory subtype at diagnosis were excluded.; b. extramedullary progression (EMP) means appearance of a new extramedullary lesion; c. classic progression (ClaP) means any one or more of the other PD criteria according to International Myeloma Working Group (IMWG) criteria. High burden refers to the percentage of BMPC > 50%. Time from the first relapse to death as overall survival (OS) after the first progression (pro-OS).
Results:
There were 268 patients included in the study, and according to their features of M protein and BMPC at progression, 206 (76.8%) patients were classified in the ClaP group, 39 (14.6%) patients in EMP group and 23 (8.6%) patients in HypoP group. The percentage of female in HypoP group was 52.2%, which was much higher than that in other two groups (36.5% in ClaP and 30.8% in EMP). In general, the patients with MM are predominantly of the IgG subtype. Interestingly, for patients featured by hyposecretion in progression, the M protein types were mainly IgA (47.9%) and light chain type (43.5%) ( P<0.001). Compared to the ClaP and EMP group, there were more patients in HypoP presenting t(11;14) (36.8% vs 16.7% vs 11.8%) and 1q21+ (70% vs 53.8% vs 53.8%) both at diagnosis and progression. And at disease progression, the proportion of patients with t(4;14) in the HypoP group was as high as 50%. Besides, in terms of clinical manifestations, HypoP patients were more likely to suffer from hypercalcemia, renal dysfunction, and lower serum M protein level and EMP experienced high level of lactate dehydrogenase (LDH) both at diagnosis and progression.
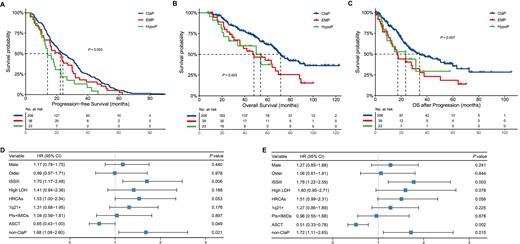
The median follow-up was 67.0m (7.6-123.0m). Figure 1 demonstrates the progression-free survival (PFS), OS and pro-OS of patients with different progression patterns. Patients in ClaP and EMP groups experienced similar PFS whereas HypoP patients had significantly shorter median PFS ( P=0.003, 23.9m vs. 22.6m vs. 14.1m). We also found that patients with ClaP and HypoP feature had inferior median OS ( P=0.007, 71.4m vs. 48.0m vs. 53.9m for ClaP vs. EMP vs, HypoP) and pro-OS ( P=0.012, 34.2m vs. 17.3m vs. 23.4m for ClaP vs, EMP vs. HypoP). Then we refer to these two as non-ClaP. In the Cox-regression, multivariate analysis showed ISS-III, ASCT and non-ClaP were associated with shorter pro-OS and OS ( Figure 1).
Conclusions:
In conclusion, our results indicate that the hyposecretory progression pattern is a valuable indicator of inferior survival. In such cases, bone marrow testing plays a crucial role in identifying and detecting this special group. Patients presenting with EMP or HypoP features tend to have a poorer prognosis, representing unmet clinical need. Therefore, it is important to recognize these particular patients as early as possible and to intensify treatment strategies.
Disclosures
No relevant conflicts of interest to declare.